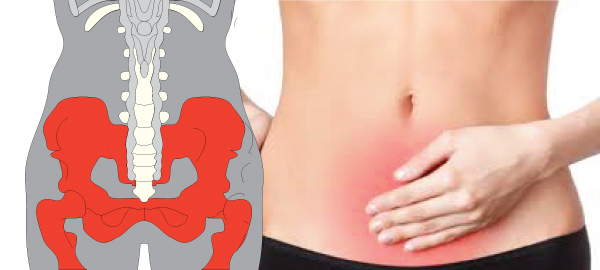
Pelvic floor disorders are diagnosed through a combination of methods that may include a medical history review, a physical examination, and sometimes specialized tests. The diagnostic process may vary depending on the specific disorder and the healthcare provider’s clinical judgment. Here are common methods used to diagnose pelvic floor disorders:
1. Medical History Review:
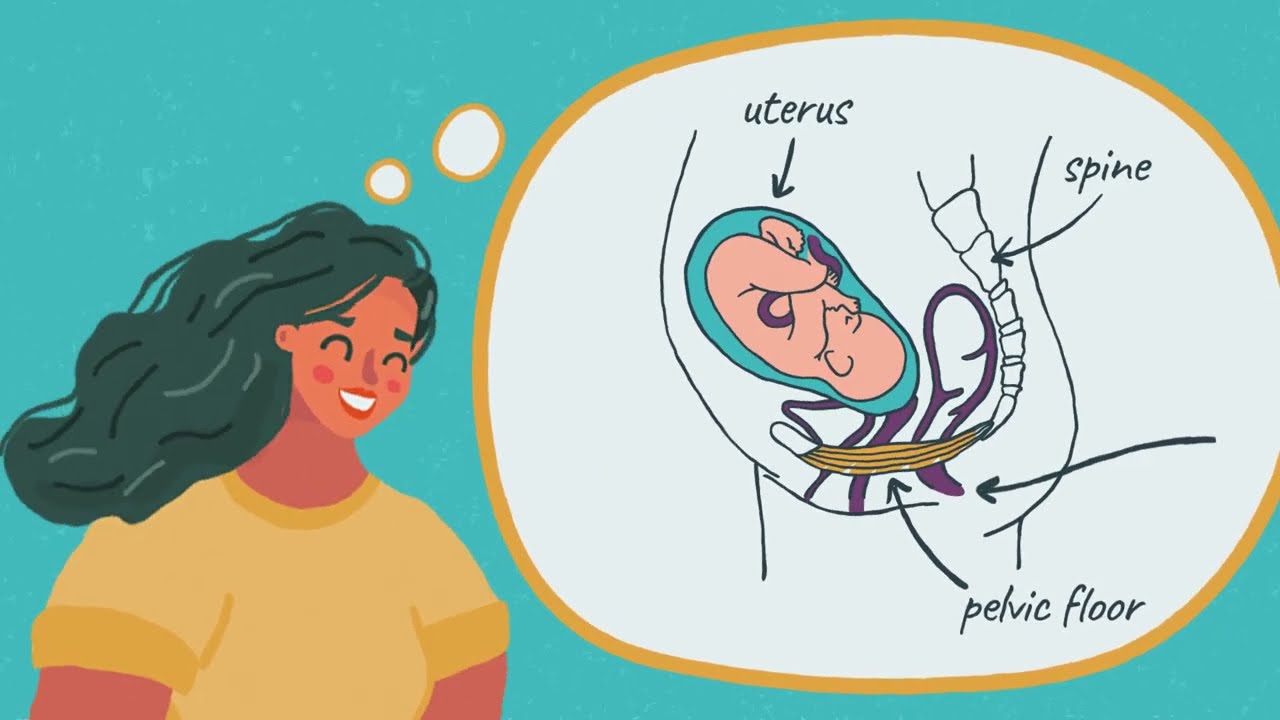
– The healthcare provider will ask you about your symptoms, including the type, duration, and severity of any pelvic floor-related issues. Information about your medical history, surgical history, pregnancies, and childbirth experiences is also important.
2. Physical Examination:
– A pelvic examination is often performed to assess the condition of the pelvic floor muscles and structures. During the exam, the healthcare provider may check for signs of pelvic organ prolapse, muscle strength and tone, and any areas of tenderness or discomfort.
3. Questionnaires and Symptom Assessment:
– You may be asked to complete questionnaires or assessment tools related to urinary incontinence, fecal incontinence, pelvic pain, or other symptoms. These tools can help quantify and categorize your symptoms.
4. Pelvic Floor Function Evaluation:
– Pelvic floor muscle function may be assessed through a physical examination, which may include palpation (feeling the muscles) and muscle strength testing. Some healthcare providers may use biofeedback techniques or electromyography (EMG) to measure muscle activity.
5. Urodynamic Studies:
– Urodynamic testing involves a series of tests to evaluate bladder function and assess how well the bladder and urethra are storing and releasing urine. These tests can help diagnose urinary incontinence and other bladder-related conditions.
6. Imaging Studies:
– Imaging tests such as pelvic ultrasound, MRI (magnetic resonance imaging), or CT (computed tomography) scans may be ordered to visualize the pelvic floor structures, assess the severity of pelvic organ prolapse, and rule out other underlying conditions.
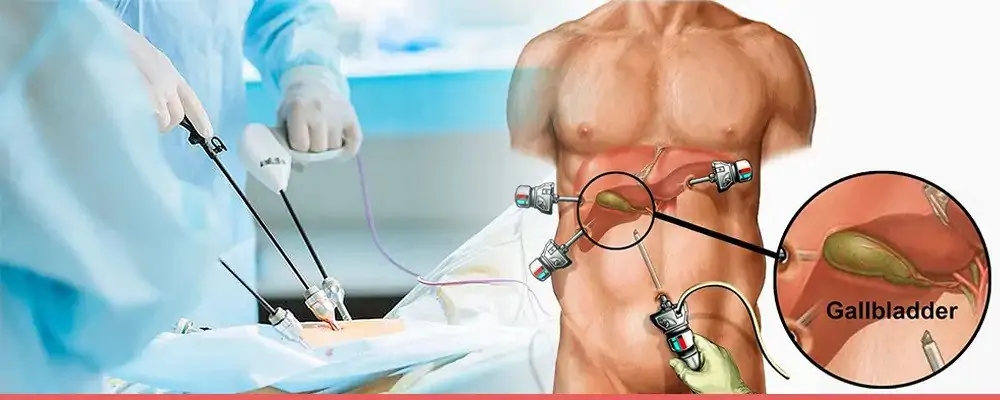
7. Cystoscopy and Urethroscopy:
– These procedures involve inserting a thin, flexible tube with a camera into the bladder (cystoscopy) or urethra (urethroscopy) to visually examine the urinary tract for abnormalities.
8. Defecography:
– Defecography is a radiologic test that uses contrast material and X-rays to evaluate the function of the rectum and anus during bowel movements. It can help diagnose fecal incontinence and rectal prolapse.
9. Colonoscopy or Endoscopy:
– These procedures may be recommended to evaluate the gastrointestinal tract if bowel-related symptoms are present, such as rectal bleeding or pain.
10. Specialized Consultations:
– Depending on the diagnosis, you may be referred to specialists such as urogynecologists, colorectal surgeons, or pelvic floor physical therapists for further evaluation and treatment planning.
The choice of diagnostic tests and evaluations depends on the specific symptoms and clinical presentation. The healthcare provider will work with you to determine the most appropriate diagnostic approach to identify and understand the underlying pelvic floor disorder. Once diagnosed, treatment options can be discussed and tailored to your individual needs.
If you or a loved one has been diagnosed with Pelvic floor disorders consult Dr. Chintamani Godbole one of the best Gastrointestinal Surgeon in Mumbai