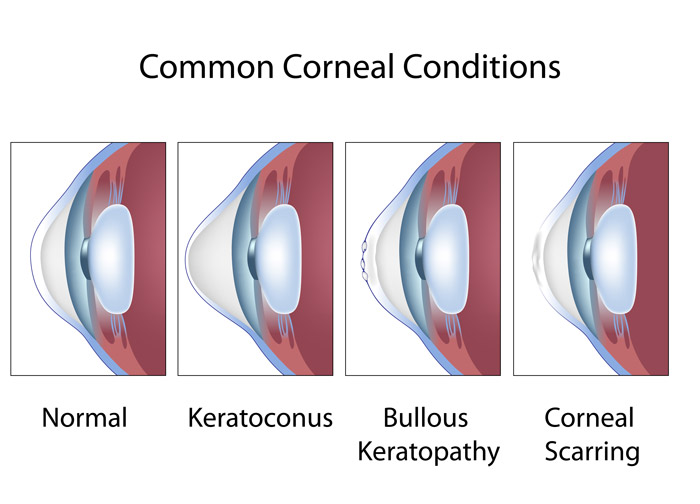
Keratoconus is a progressive eye disorder that affects the cornea, which is the clear, dome-shaped front surface of the eye. In individuals with keratoconus, the cornea gradually thins and bulges outwards into a cone-like shape, leading to distorted and blurred vision. This condition can cause significant visual impairment and discomfort.
Key characteristics of keratoconus include:
1. Corneal Thinning: The cornea, which is normally round and smooth, becomes progressively thinner in the center. This thinning weakens the corneal structure and allows it to bulge outward.
2. Cone-Like Shape: As the cornea bulges, it takes on a cone-like shape. This irregular shape causes light entering the eye to be improperly focused, leading to distorted and blurred vision.
3. Visual Disturbances: Individuals with keratoconus often experience changes in vision that can include blurred or distorted images, multiple images (ghosting), glare, and light sensitivity. These visual disturbances can significantly impact daily activities and quality of life.
4. Onset and Progression: Keratoconus typically begins during adolescence or early adulthood. The progression of the condition can vary, with some individuals experiencing rapid changes in corneal shape and vision, while others have a more gradual progression.
The exact cause of keratoconus is not fully understood, but it is believed to involve a combination of genetic, environmental, and hormonal factors. Some factors that may contribute to its development include:
– Genetics: There is often a genetic predisposition for keratoconus. Individuals with a family history of the condition are at a higher risk.
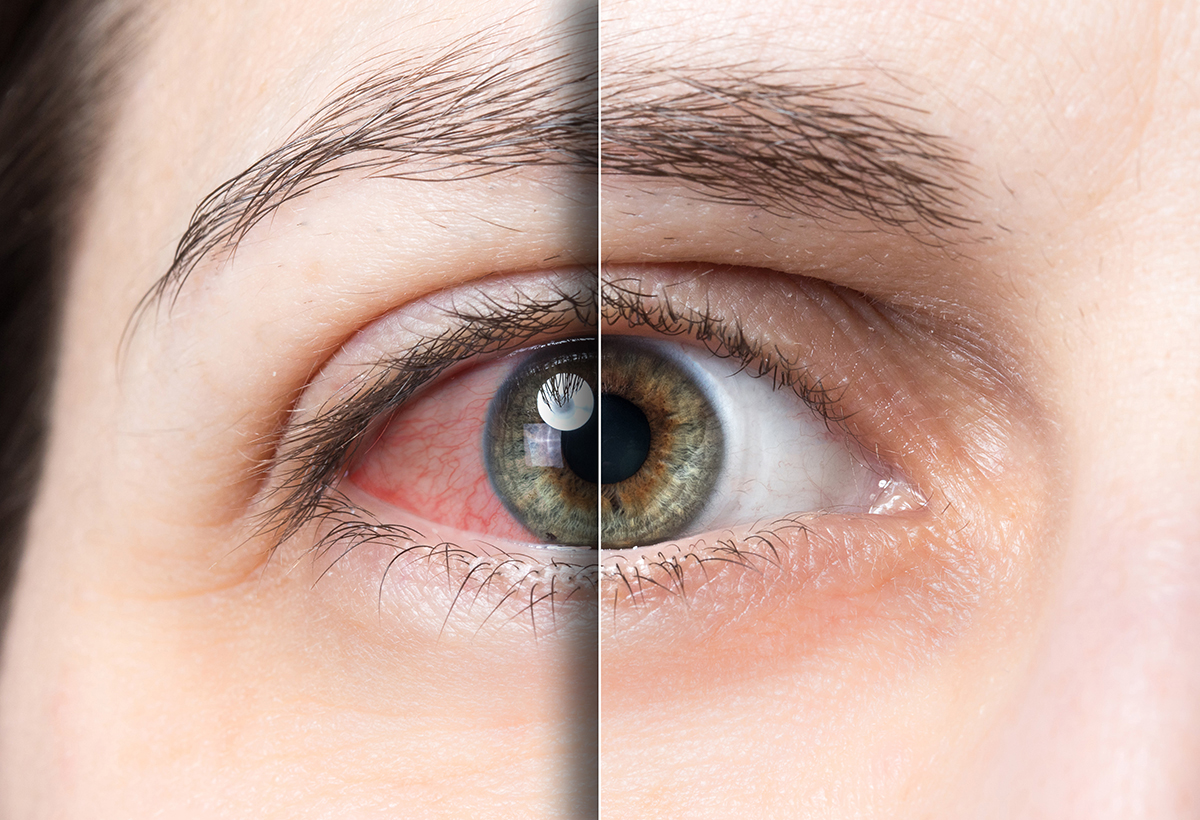
– Eye Rubbing: Frequent and vigorous eye rubbing may contribute to the thinning of the cornea and the development of keratoconus.
– Hormonal Changes: Hormonal changes during puberty and pregnancy have been suggested as potential triggers for the condition.
– Eye Allergies: Chronic eye allergies and inflammation could play a role in the development or progression of keratoconus.
– Weak Collagen Cross-Linking: Collagen cross-linking is a natural process that helps maintain the cornea’s strength. In keratoconus, the cross-linking process may be weakened, contributing to corneal thinning.
Treatment options for keratoconus depend on the severity of the condition. In the early stages, corrective eyeglasses or soft contact lenses may help improve vision. As the condition progresses, specially designed rigid gas permeable (RGP) contact lenses or scleral lenses may be used to provide better visual correction by masking the irregular corneal shape.
In cases where vision cannot be adequately corrected with contact lenses, surgical options may be considered, such as:
– Corneal Collagen Cross-Linking (CXL): This procedure involves applying riboflavin (vitamin B2) eye drops to the cornea and then exposing it to ultraviolet light. CXL aims to strengthen the corneal structure and slow or halt the progression of keratoconus.
– Intacs or Corneal Ring Segments: These are small, semi-circular plastic inserts that are surgically placed in the cornea to help reshape it and improve vision.
– Corneal Transplant: In severe cases where vision is significantly impaired, a corneal transplant (keratoplasty) may be necessary. During this procedure, a damaged cornea is replaced with a healthy donor cornea.
Early detection and management are crucial in controlling the progression of keratoconus and preserving vision. If you suspect you have keratoconus or are experiencing vision changes, it’s important to consult an eye care professional for a comprehensive eye examination and appropriate treatment recommendations.
ophthalmologist Dr. Sonia Maheshwari , Eye specialist in Vikhroli for a proper evaluation and guidance on the most appropriate treatment plan. she is practicing at Clear Sight Eye care and Laser Center.