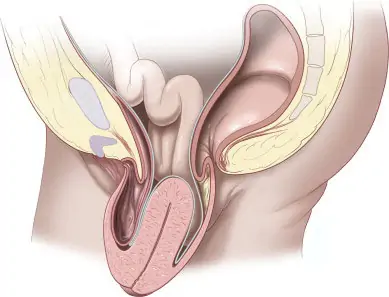
Surgery for pelvic floor diseases is typically considered when non-surgical treatments have been ineffective or for severe cases that significantly impact a person’s quality of life. The decision to recommend surgery is based on the specific type of pelvic floor disorder and its severity. Here are some situations in which surgery for pelvic floor diseases might be recommended:
- Pelvic Organ Prolapse (POP):
- Severity: If the prolapse is severe and is causing significant symptoms, such as a bulging sensation or pressure in the pelvic area.
- Impact on Function: When pelvic organ prolapse affects a person’s ability to perform daily activities or interferes with bladder, bowel, or sexual function.
- Urinary Incontinence:
- Failed Conservative Treatments: When non-surgical approaches, such as pelvic floor exercises, behavioral therapies, or medications, have not provided sufficient relief.
- Severe Symptoms: In cases of severe stress incontinence or urge incontinence that significantly impact quality of life.
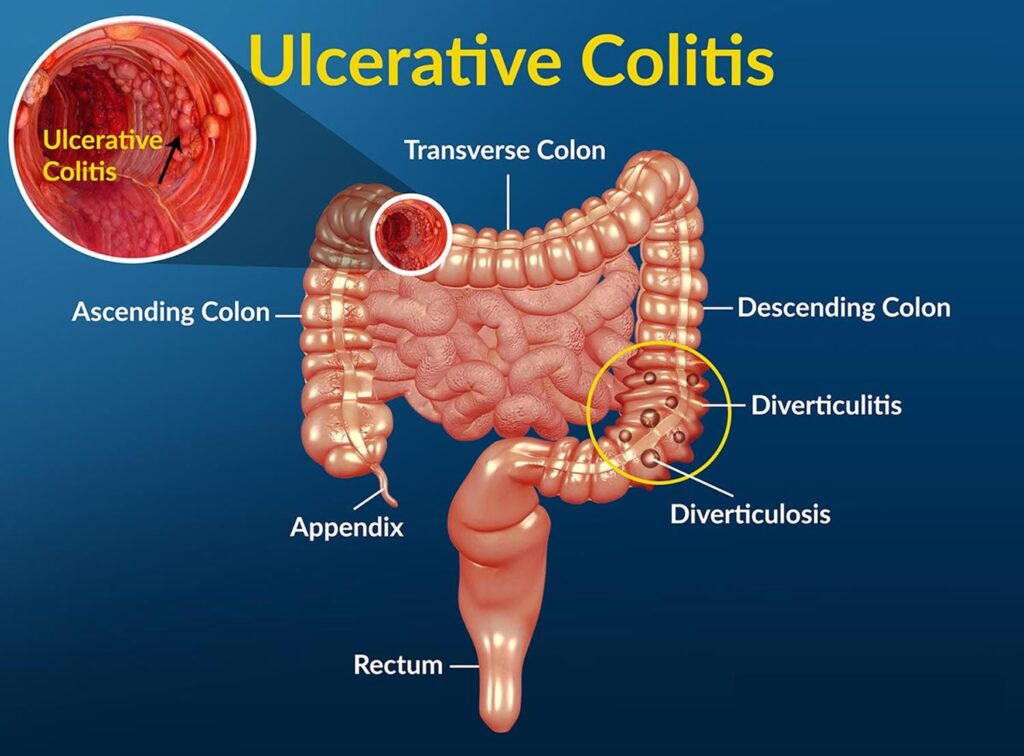
- Fecal Incontinence:
- Ineffectiveness of Conservative Measures: If non-surgical interventions, such as dietary changes, medications, or pelvic floor exercises, fail to improve symptoms.
- Significant Impact on Daily Life: When fecal incontinence has a profound impact on a person’s ability to participate in normal daily activities.
- Pelvic Floor Dysfunction:
- Symptom Severity: In cases where pelvic floor dysfunction is severe, causing persistent and debilitating symptoms.
- Failure of Conservative Approaches: When conservative treatments, including physical therapy and lifestyle modifications, have not been successful.
- Recurrent Infections or Complications:
- Recurrent Infections: For conditions like recurrent urinary tract infections associated with pelvic floor dysfunction.
- Complications: If complications, such as recurrent urinary retention or kidney problems, arise due to pelvic floor disorders.
It’s crucial to note that surgery is not the first-line treatment for most pelvic floor disorders. Conservative measures, such as physical therapy, lifestyle modifications, and medications, are often explored first.
The decision to undergo surgery should be a collaborative one between the patient and the healthcare team, considering the individual’s overall health, preferences, and the potential risks and benefits of the surgical intervention.
A thorough evaluation and discussion with a urogynecologist or pelvic medicine specialist are essential to determine the most appropriate course of action. Embark on a journey to digestive well-being with the expertise of Dr. Chintamani Godbole, a distinguished Gastrointestinal Doctor in Mumbai.